Umbilical cord blood
For centuries, the umbilical cord and the blood left in it (cord blood) were discarded as medical waste. But, today, we know that cord blood is one of the richest sources of stem cells, specifically hematopoietic stem cells.
Hematopoietic stem cells are early-stage cells that have the potential to produce all other types of blood cells. They have been used to cure blood-related diseases with stem cell transplants for over 30 years.
Not only that, but studies also show that cord blood can be used to detect a babies’ illness early, and cord blood stem cells are being explored as a potential therapeutic over 80 other genetic and blood-related diseases.
Cord blood banking
Knowing the benefits, deciding to preserve your baby’s cord blood is easy. And if you do, your doctor will collect the cord blood after the baby is born. The whole process is minimally invasive and painless. You do not need to make any special modifications to your birth plan.
What happens when your sample arrives in the lab, on the other hand, is quite complex. It involves separating and collecting stem cells, quality checks to ensure the sterility, viability (ability to grow), and sometimes stem cell typing, which looks at markers on the surface of the stem cells that are used for stem cell matching.
How variability between cord blood samples affect banking
All of the steps involved in collecting, processing, and preserving cord blood are standardized. But this does not mean that there won’t be variation between baby-to-baby on the amount of cord blood collected, and the number of stem cells in the cord blood sample.
Studies also show that factors like the birth weight of the baby, size of the placenta, the volume of cord blood collected, and the delivery methods (cesarean vs. vaginal delivery, for example) can impact the total number of cells in cord blood samples.
Factors affecting bankability
Sample variability is a problem because low blood volumes and a reduced number of cells can make a percentage of collected samples unsuitable for banking. In this paper, scientists refer to this as ‘bankability’ or the probability of banking, which takes into account how useful a cord blood sample will be for future use in terms of a transplant or research use.
The study aimed to look at all possible factors that could affect the bankability of a cord blood sample, particularly ones that can be adjusted to increase the likelihood of samples being banked. Some of the factors considered included the size of the placenta, weight of the baby, APGAR scores, amount of liquid given to the mother during the delivery, and the delivery method.
Size and delivery method matters
The researchers looked at 869 cord blood samples banked over 15 years, from 1999 to 2015. All babies were born after 35-weeks of gestation, and the cord was clamped 60 seconds after birth. Only samples with a total volume of 91mL (milliliters) were included in the final analysis.
Also, in terms of storage, only samples with more than a billion cells were processed and cryopreserved.
In agreement with previous research, they found a link between higher placental weight and vacuum-assisted vaginal deliveries. The likelihood of having more than a billion cells per sample (and the bankability) was higher with bigger placentas and with vacuum-assisted delivery.
They also found a link between bankability and the amount of liquid administered to the mother. The bankability decreased by about 30%, with each 500mL of liquid infused. It was hypothesized that hemodilution, where the number of cells is diluted or reduced as a result of an increase in the amount of liquid, may be responsible.
Predicting bankability
The researchers were also able to generate a chart (called a nomogram), which can now be used to predict the bankability of a cord blood sample. As you see below, the chart is based on the three variables they found were linked to bankability. The hope is, as research into this field grows, we can identify more and more external factors that can be managed by delivery teams to increase the likelihood of your baby’s precious stem cell sample from being preserved.
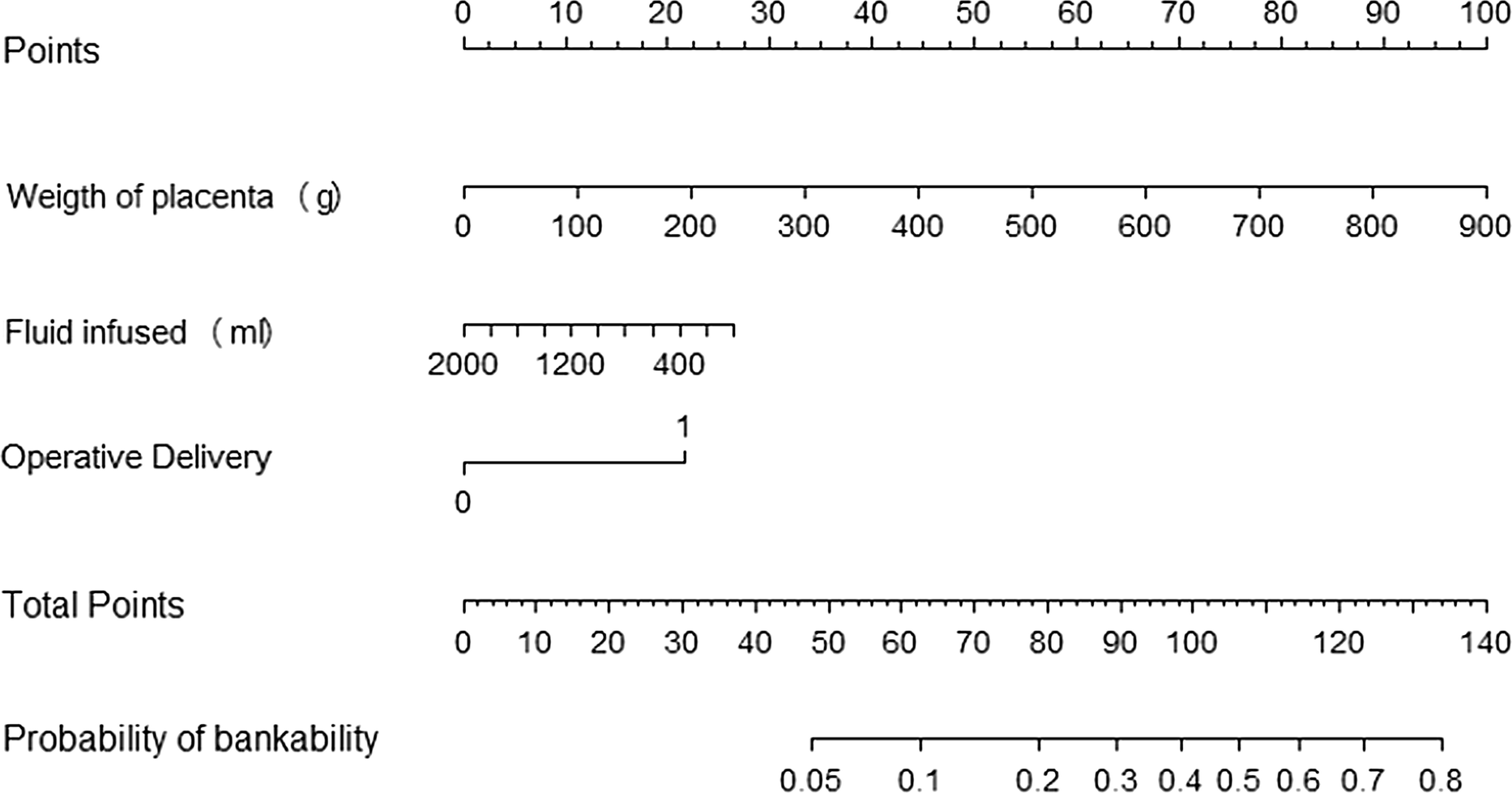
Nomogram for computing the probability of bankability from the multivariable logistic model. The probability of bankability can be derived as follows: partial probability scores relative to each predictor (weight of placenta, mL infused and operative delivery) are read on the upper scale. Their sum is then reported on the total score scale and the corresponding probability is obtained on the lower linear predictor
Reference
Factors associated with blood cord unit bankability: an analysis of a 15-year-long case series